Credentialing services
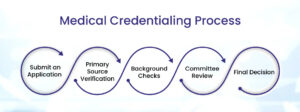
- We assist healthcare providers in enrolling with insurance networks, including commercial insurance companies, Medicare and Medicaid. Our credentialing team thoroughly reviews and completes the necessary applications, ensuring that all required information is accurately and comprehensively provided. We proactively track the progress of your enrollment, working closely with insurance companies to expedite the process.
- Our experts meticulously gather, verify, and submit all necessary documentation required for provider credentialing. This includes verifying licenses, certifications, education, training, work history, and professional references. We ensure that your credentials are up to date and meet the specific requirements of each insurance network, ensuring a smooth credentialing process.
- Credentialing is an ongoing process that requires regular updates and re-verification. We manage the re-credentialing process, ensuring that all required documents are submitted in a timely manner to maintain your active status with insurance networks. Our team proactively tracks re-credentialing deadlines and sends reminders, ensuring that your credentials are always current and compliant.
- We assist providers with the registration and management of their Council for Affordable Quality Healthcare (CAQH) profiles. We ensure that your CAQH profile is accurately completed and regularly updated with the latest information, including licenses, certifications, and practice details. This enables streamlined data exchange between you and insurance companies, reducing administrative burden and improving efficiency.Our credentialing services extend beyond enrollment to include insurance contract negotiation. We work with you to review, negotiate, and secure favorable insurance contracts with insurance companies. Our team leverages industry knowledge and experience to ensure that you achieve fair reimbursement rates and favorable contract terms, maximizing your revenue potential.
- We assist in maintaining ongoing compliance with insurance networks and regulatory requirements. Our team stays up to date with changes in credentialing and enrollment standards, ensuring that your practice remains compliant. We proactively monitor expiring credentials and deadlines, providing timely reminders and support to keep your practice running smoothly.
Partner with 110techs Medical Services for streamlined and reliable credentialing services that enable seamless practice operations. Let us handle the administrative complexities of provider enrollment, credentialing, and compliance while you focus on delivering exceptional patient care. Contact us today to discuss how our credentialing services can be tailored to meet the unique needs of your practice.
 info@110tech.com
info@110tech.com Texas, United States
Texas, United States